In case you were wondering what a typical day in the life of a Veterinary Nutrition Specialists is like, my working days are mostly filled by those with chronic diseases: diabetic cats with kidney disease; dogs with food allergies and pancreatitis; maybe a diabetic dog with food allergies, history of pancreatitis, kidney disease, AND a picky appetite just to make it interesting. But on one particular day a few years back my first appointment of the morning was a little different. The reason for the visit as listed in the medical chart was “questions about preventing cancer” and my soon-to-be patient was a 4 month old Golden Retriever puppy full of happy, healthy, fluffy, puppy cuteness.

Not an actual picture of my patient, but just as cute.
After introducing myself to the puppy and his people I quickly learned what brought them in seeking cancer prevention advice. Turned out that this particular puppy was the fourth in a series of GoldenS cared for by the owners over the previous 20+ years. The first died at 10 years of age from hemangiosarcoma (an aggressive cancer of blood vessels that usually starts in the spleen and quickly spreads in the body), the second at age 6 from osteosarcoma (an aggressive cancer of the bone that usually starts in one bone and can spread throughout the body), and the third died at 2 years of age from lymphoma (an aggressive cancer of one of the white blood cell families, that can go and do whatever it wants). Their most recent loss was less a year before our appointment, so needless to say, this couple was very concerned about losing this new puppy too soon. They wanted to know if there was anything they could do diet and supplement-wise to prevent cancer from striking another four-legged family member.

Another gratuitous puppy picture.
If any of my readers were wondering that same thing, the short answer was no. There are no proven dietary changes or nutritional supplements that have been definitively shown to prevent cancer in dogs and cats. Cancer is a leading cause of death in dogs and cats with genetics, viruses, environmental toxins, age, and neuter status all having a direct or indirect role in the development of certain types of cancer.
So what do dog and cat caregivers need to know about cancer and possible nutritional prevention/treatments?
#1: What causes cancer?
Cancer results from damage to DNA (the genetic code of every cell) that 1) allows that cell to replicate itself unchecked, 2) to avoid normal housekeeping systems that would otherwise destroy an abnormal cell, 3) to induce new blood vessels growth to supply the cancerous cells with nutrients, and 4) to spread either locally or distantly (or both).
Cancer incidences are higher in certain pure-bred dogs than in mixes; viruses such as feline leukemia virus (FeLV) and transmissible venereal tumors (TVT) can induce cancer development and are acquired by close contact with infected animals; unneutered male dogs can develop testicular tumors just as unneutered females can develop uterine cancer (the risk of these two tumor types is virtually eliminated with neutering); cats and dogs living in households with heavy smokers have an increased risk of oral and nasal cancers due to environmental tobacco exposure. Additionally dogs and cats today are living longer thanks to vaccines, complete and balanced commercial diets, and advances in medical prevention/treatment of other diseases. Essentially, by preventing other potentially fatal diseases we have opened up the playing field for cancer in older aged dogs and cats.
Breed predispositions play an especially important role in cancer occurrence in Golden Retrievers. Goldens are beautiful, smart, dedicated family dogs, steadfast companions, but they are also a breed that has among the highest risk for cancer development at any age. This is one of the primary reasons for the development of Golden Retriever Lifetime Study. This study enrolled 3000 young Goldens and will track the genetics, environment and diet of each individual dog to help identify risk factor and possible prevention strategies for cancer as well as other chronic disease. This is a huge undertaking not only by the researchers, but the family committing their beloved canines and their own time to this study. At the time of my puppy appointment, the Golden Retriever Lifetime Study had not yet been launched and it will be at least a decade, if not longer, before we have any inkling of results.
What can dog and cat caregivers do about these risks? If you are adopting a purebred dog or cat, learn about the breed and what conditions can typically affect that breed. Do your research on any potential breeders as well. Find out what steps (if any) they are taking to screen their breeding pairs for known and potential health problems. Is the breeder tracking disease incidences (including cancer occurrence) in their lines? Once that cat or kitten is in your care, vaccinate for FeLV, if they are considered to be at-risk for this disease. Since FeLV is a “social” virus that required direct contact with an infected cat, indoor only cats in a FeLV-free household don’t typically need annual boosters. But talk to your veterinarian about your individual cat’s risk before stopping any vaccine regime. Canine TVT is a sexually transmitted disease, and both testicular and uterine tumors require intact reproductive tracts so the best way to prevent all of these is by neutering your dog. And if you are a smoker who hasn’t/can’t/doesn’t want to end their habit, at least smoke outside away from your dog or cat.

Old age happens, but it’s better than the alternative.
#2: What about specific foods and cancer risk?
If you are reading my posts, you are interested in canine and feline nutrition and have likely read other websites that claim that “kibble causes cancer” or that there are “cancer causing preservatives in pet food”, but scientific evidence for these claims is very much lacking. These claims are also almost always made by either a distraught pet owner looking for someone to blame for unexpected cancer diagnosis or by a person or business trying to market their own special line of “miracle cure-alls.” Our old Labrador, Maggie, lived 14 ½ years eating primarily dry dog food (with the occasional pizza or bread roll stolen from the counter when we weren’t looking), and ultimately died from a stroke-like event that hit her one morning. My 18-year-old cat Oliver is asleep next to me right now, has eaten dry commercial food his whole life and, other than his arthritis, is the picture of geriatric health; while our 3-year-old cat Cosette had eaten a variety of canned and dry foods over her short life, loved eating cat grass (that I grew myself) every day, and just died from transitional cell carcinoma in her left kidney (a rare cancer in cats, let alone in one so young). I don’t blame Cosette’s once-a-day cat grass habit for her developing cancer nor do I attribute Oliver’s longevity and health to dry food; cancer happens even to good cats and dogs.
But what does the vet literature say? There are some published veterinary studies that have tried to find an association between specific food intakes and cancer risk. One study looked at feline oral squamous cell carcinoma and another looked at thyroid adenomas in cats, but both of these studies relied on owners to report frequency and types of foods given over years to decades prior to the cancer diagnosis. Another study in dogs tried to draw a connection between intake of fresh fruits and vegetables with lowered risk of transitional cell carcinoma in Scottish Terriers. Again, these researches relied on owners to recall types and amount of fresh produce fed over the previous years. Most people can’t recall how much fruit and veg they fed themselves over the last week, let along how much they fed their dogs. I’ve worked with people who can’t even remember the name of the food they use (“it’s the purple bag with black writing”) or live in household with multiple feeders (intentional and unintentional). Recall bias is essentially the over- or under-reporting of foods and lifestyle habits that a responder thinks may be associated with a particular disease state. Recall bias is a significant enough problem in human health studies that nutritional epidemiologists have almost completely abandoned this method of data collection, yet for some reason veterinary researchers still rely on it. Food recall is always faulty in my clients, and they are highly motivated to remember their dog or cats food intake. To date, any veterinary study using only caregiver food recall to draw conclusions about diet and cancer risk in dogs and cats should be taken with a heavy dose of skepticism.
What do cat and dog owners need to know about commercial diets and cancer risk: Improvements in disease prevention, nutritional needs, medical care, and diagnostics mean that today’s cats and dogs are living to ages when accumulated DNA damage can result in cancer. Feed a complete and balanced diet that meets your individual animal and family’s lifestyle needs. If you want to feed a varied diet or a portion of fresh foods on a regular basis, that is no problem, as long as the overall diet still meets your dog or cats nutritional needs, they tolerate it well, and the foods selected are not harmful (no toxic foods like garlic or grapes, and avoid feeding foods that contain Salmonella or Campylobacter).

The wild ‘carnivore’ back from the hunt.
#3: What about the role of obesity in cancer development?
This may be the one area of nutrition and health that could impact disease prevalence. In people, obesity has been shown to increase risk of specific cancers, such as uterine, liver, and post-menopausal breast cancer. These same associations haven’t been seen in dogs or cats, but calorie restriction has been shown to decrease cancer risk in rodent and primate models. The only published prospective (meaning they started with healthy dogs and followed them forward in time) study in dogs to date that looked at lifetime intakes and disease prevalence showed an equal number of cancer occurrences in lean and overweight dogs, but the small sample size (only 48 dogs in total) make this comparison almost meaningless. The results of the Golden Retriever Lifetime Study may give us more insight into this question.
What do cat and dog owners need to know about obesity and cancer risk: Lack of scientific data doesn’t mean that there is not an association between obesity and cancer development in companion dogs and cats, it just means that we don’t have a study that could answer this question. Even in the absence of a clear link between obesity and cancer, excess weight is a proven risk factor for other problems in dogs, and cats including joint disease, diabetes, skin disease, breathing difficulties, and at least in dogs has been shown to decrease longevity.

There may be less to love, but you can love them longer.
#4: What about the role of carbohydrates and cancer?
A quick Google search on “carbohydrates and cancer” will give pages of websites claiming to prevent or cure cancer by avoiding carbohydrates, and especially carbohydrates that include GMOs and gluten (the “evil” ingredients du jour). And there is big money in making these kinds of diet claims. Just look at the recent Belle Gibson story. Her fake cancer and food cure story garnered her hundreds of thousands of followers (and dollars), spawned a book, an app, and stories in international magazines, until she was recently exposed as a fraud and a thief.
There is one veterinary study that the anti-carb people like to point to and shout, “See, carbohydrate influence cancer!” It was published in 2000 and looked at response to cancer treatment in dogs with lymphoma fed a low carbohydrate (18% of the calories) diet supplemented with fish oil and arginine. Low carb advocates (including one of the lead authors) have cherry-picked the results of this study to make claims like “dogs with cancer should be fed a low carbohydrate diet” and “carbohydrates feed cancer” (emphasis is mine), yet when you read the entirety of the paper you learn that the control diet (the non-supplemented diet used as a comparison for the supplemented diet) had the exact same carbohydrate content as the study diet, just no fish oil and extra arginine. And the low carb control diet had absolutely no influence on cancer progression relative to expected outcomes. Again, feeding a low carbohydrate diet alone made no difference in disease free interval or survival time in these dogs with lymphoma. Yes, cancer cells utilize blood sugar (glucose) more rapidly than the surrounding normal cells, but this happens whether the individual consumes carbohydrates directly in their diet or if the blood glucose is produced from glycogen (a type of carbohydrate stored in the muscle and liver) or from gluconeogenesis (production of glucose in the liver) from metabolism of fatty acids and amino acids (building blocks of protein). The body of an adult, non-reproducing, non-lactating animal is very good at maintaining blood sugar levels, even when fed a carb-free diet. Additionally, there is not a single veterinary study that has demonstrated that dogs or cats fed low to no carbohydrate diets have less cancer incidence than dog or cats fed moderate to high carbohydrate diets. Not that I am advocating that dogs and cats should be fed lots of starches and simple sugars, I just don’t want people to wave the cancer prevention/treatment flag when touting the “benefit” of a carbohydrate-free diet.
What do cat and dog owners need to know about carbohydrates and cancer risk: At this time there is no evidence that a diet with a low (less than 20% of the calories), moderate (20-40% of the calories), or high (greater than 40% of the calories) carbohydrate content has any bearing on cancer development in dogs and cats. There may be other reasons to feed a reduced carbohydrate diet, like management of feline diabetes, and animals with insulin secreting tumors (insulinomas) will often benefit from a reduction in overall carb intake, but like for all conditions the specific diet selected for your dog or cat should encompass their whole health needs.

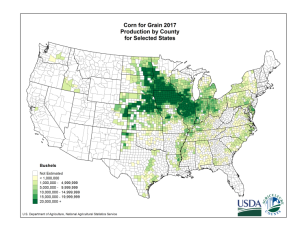
Psst, no one told her she wasn’t supposed to like corn.
#5: What about antioxidants for cancer protection?
The most common supplements marketed for “cancer prevention” or “cancer treatment” include combinations of antioxidant compounds, such as vitamin C, vitamin E, carotenoids, and selenium. On the surface this may seems to make sense. Antioxidants exist within each cell to balance and prevent the accumulation of reactive oxygen species (ROS) that are formed during normal cellular metabolism. These ROS can have damaging effects on nearby DNA, effects that could potentially end up in cancer development. The balance between formation of ROS and antioxidant capacity of the cell is dependant on dietary intake of antioxidants compounds, as well as the demand on the antioxidant systems through exposure to oxidative damage. So supplementing antioxidants seems like a smart thing, right? Maybe not. In people increased intake of antioxidants may influence cancer development, but not in the way we want. Prospective studies in people have shown that supplementing beta-carotene and vitamin A may increase the risk of lung cancer in smokers; high dosage vitamin E may increase prostate cancer risk; and women (but not men) taking high dosages of vitamins C and E, selenium and zinc, may actually be at an increased risk of skin cancers. And there are a number of other studies looking at different cancer that have shown no effect (good or bad) of antioxidant supplementation. It is important to note that these studies in people were based on longer term (5-15 year studies) using tens of thousands of individuals. Veterinary medicine hasn’t done anything like this, until the Golden Retriever Lifetime Study and even that would be considered small by human study stanards. There are no published studies evaluating specific antioxidant supplementation and cancer prevention in dogs and cats, though increased antioxidant intake in older dogs may help protect cognitive ability.
What do cat and dog owners need to know about antioxidants and cancer risk: There is no evidence that increased intake of antioxidants will prevent cancer in dogs and cats, and if anything, the studies in people have demonstrated that megadoses (10-100X normal dietary requirements) of certain antioxidants may actually increase risk of certain cancers. Antioxidants consumed as part of a healthy, balanced diet are fine, as are naturally occurring antioxidants found in fresh fruits and vegetables (non-toxic ones of course). There may also be some benefit to cognitive function with moderate increases in antioxidant intake in middle age to older dogs and cats.

It is all about finding the right balance (and avoiding known risks).
The bottom line…
There are no proven dietary strategies or techniques to prevent cancer development in dogs and cats. Defects in tumor suppressor genes, exposure to environmental toxins, obesity, and chronic inflammation have been proposed as causes of tumor development in people and many of these same mechanisms may occur in dogs and cats. Genetic factors and environmental toxins may not be avoidable or preventable, but avoiding obesity and feeding a complete and balanced (no deficiencies, no excesses) are within every caregiver’s control.
Happy Feeding!
Lisa P. Weeth, DVM, MRCVS, DACVN