Ah, the pancreas… an often overlooked and misunderstood part of the digestive system that only gets noticed by veterinarians and caregivers when it’s not working well. But the pancreas shouldn’t just get attention when it is inflamed and painful (from Pancreatitis), or not producing enough insulin (from Diabetes Mellitus), it deserves recognition for doing its job well and not causing problems on a day-to-day basis. Today’s post is to familiarize you with the pancreas and (hopefully) give you a few tips to help you keep it happy for years to come.

Happy Pancreas = Happy Dog
Anatomy of the Pancreas
This part gets a bit technical, so bear with me. The pancreas is a glandular organ that sits behind the stomach and extends across the length of the stomach to the upper small intestinal (the duodenum). It connects to the duodenum via the pancreatic duct, which serves at the pathway for release of digestive enzymes and other essential compounds into the intestinal tract. This part of the pancreas’ job is called its exocrine function. This is in addition to the pancreas’ other, probably more familiar role, the production and release of insulin into the blood stream (i.e., its endocrine function). The endocrine pancreas will be covered in my next post on Diabetes Mellitus; I’m not completely ignoring that topic, just pushing off for now.
Pancreatic enzyme release is triggered by the hormone cholecystokinin (CCK) that is secreted from the intestinal cells in response to the intake of certain food components, specifically protein and fat. Both protein and fat will stimulate CCK release, but fat has a much more pronounced effect even at lower intakes. Irrespective of trigger, the secretion of CCK causes the pancreas to contract and squeeze pancreatic enzymes down the pancreatic duct and into the duodenum to begin the breakdown of dietary macronutrients (macronutrients = dietary protein, fat and carbohydrate). There are a few other functions of CCK, such as stimulating contraction of the gall bladder and creating a feedback on the brain to slow food intake, but it’s CCK’s effect on the pancreas that I am focusing on for management (and minimization) of pancreatitis.
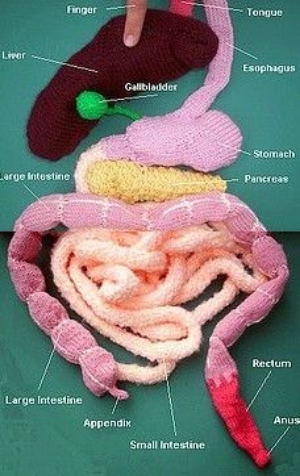
Your key digestive organs, without the actual blood and guts
The Exocrine Pancreas
The primary exocrine enzymes produced by the pancreas are trypsin and chymotrypsin (both used for protein digestion), lipase (required for fat digestion), and amylase (essential for starch digestion). These enzymes are produced in their inactive forms, which must be activated by other enzymes in the presence of bicarbonate (also made in the pancreas). For example, trypsin is actually made and stored in the pancreas as trypsinogen. Trypsinogen is packaged into zymogen granules within the pancreas and kept separate from bicarbonate. This isolation of enzymes and activators protects both the integrity of the digestive process and the pancreas itself. If trypsin becomes activated too early not only will it not get into the duodenum where it is needed for food digestion, but it will start to digest the proteins in the pancreas instead. And this is painful. Very, very painful.

One of my former patients on IV nutritional support, fluid support and pain meds because of severe pancreatitis.
What Causes Inflammation of the Pancreas?
The clinical name for inflammation in the pancreas is pancreatitis (pancreas- = pancreas + -itis = inflammation). Pancreatitis can either be acute (vomiting and pain within hours) or chronic (low smoldering illness with vague signs that can be confused with other medical conditions).
In dogs, one of the most common dietary causes of acute pancreatitis is eating a non-food item (like 2 lb of bird seed) or eating fatty table scraps (either intentionally fed or found by rooting through the garbage). The exact mechanism of pancreatitis isn’t known but it is believed that the higher than normal fat intake causes the rapid increase in circulating blood fats and then “activation” of pancreatic enzymes within the pancreas. Other risk factors for acute pancreatitis include being a miniature Schnauzer or Yorkshire terrier (sorry pups), or any other dog breed that has a genetic predispositions to hypertriglyceridemia (the term for high circulating levels of triglyceride in the blood); being on medication such as potassium bromide and phenobarbital (two common anti-seizure medication); and being more than 20% over your ideal weight (yep, being a fat dog isn’t a cosmetic issue). Chronic pancreatitis in dogs is a bit more challenging to identify as the clinical signs can be vague and are often confused with other chronic medical conditions, because of this chronic pancreatitis is thought to be an under-diagnosed and under-reported condition. One study out of the UK conducted post-mortem evaluations of 200 dogs that had died from a variety of different causes (none of which were reported to be either acute or chronic pancreatitis in the medical records by the way) and found evidence of chronic pancreatitis in one-third of them.
Cats on the other hand like to be different. Genetics, medications, obesity, and high fat meals are not often associated with pancreatitis in cats. Instead stressful events, like introduction of a new animal into the household or having work done at your home, seem to be the more common histories among cats that present to their veterinarian with signs of acute pancreatitis. Many of these cats may also be diagnosed with what veterinarians like to call triaditis, (triad- = three + -itis = inflammation), meaning they are found to have evidence of inflammation in the pancreas (pancreatitis), in the liver (hepatitis), and in the intestinal tract (enteritis) all at the same time. Chronic pancreatitis can also be seen along with diabetes mellitus in cats, though just like with triaditis it often becomes a chicken-or-the-egg game to figure out which came first.
What Does Pancreatitis Look Like?
Animals, both dogs and cats, with mild cases of pancreatitis may vomit, refuse food, or seem quieter than usual at home. Dogs and cats with chronic, low-grade pancreatitis may have vague signs such as an intermittently poor appetite and weight loss. Severe pancreatitis can cause not only vomiting, food refusal, and lethargy, but diarrhea, fever, and abdominal pain. Severe pancreatitis, if left untreated, can also result in shock, circulatory collapse, and death. So pancreatitis is basically badness, followed by more and more severe badness if not caught and treated.

Signs of pancreatitis aren’t always obvious.
What Can We Do About It?
Supportive treatment for dogs and cats with pancreatitis is very similar: IV fluids to keep them hydrated, anti-nausea meds to stop them from vomiting, and pain control (whether they are acting overtly painful or not) will be on the list. Dietary therapy on the other hand is less consistent so here is where I’d like to provide some general guidelines to caregivers, vet techs, and veterinarians when treating dogs and cats with known or suspected pancreatitis.
The two most important features of a diet for an animal with pancreatitis are (in order of important): 1) feeding a diet that is LOWER in fat than what was being fed before and 2) feeding a diet that is MORE digestible than what was fed before. If you don’t know what is causing the GI signs you’re seeing and you have pancreatitis as one of the possible causes on the list, err on the side of caution and just feed a lower fat, more digestible diet. Seems straight forward but I see a lot of confusion in practice about how to translate this to an actual diet so I give you…
Dr Weeth’s Dietary Consideration for Feeding Animals with Pancreatitis

What is in that bowl is as important as the rest of the medical treatment
- Dietary fat is a wonderful thing for healthy animals, except when it’s not. Fat can enhance the palatability of the food (I much prefer half and half in my coffee to skim milk); in the right amounts and with the right fatty acid profile can improve coat glossiness and decrease shedding (and big dogs can shed a lot!); fat also provides more calories per gram than either protein or carbohydrates, so feeding a higher fat diet relative to a moderate or low fat diet will increase energy density, reducing the overall volume of food needed each day; and with this reduction in volume in, so, too, do you see a reduction in the volume of poop coming out. The end result of feeding a higher fat food is often that the dog or cat readily eats their food, has a lovely shiny coat, doesn’t shed very much, and has a low stool volumes. Sounds perfect (and a lot like the reasons people give for feeding raw … hhmmm… maybe it’s not the “raw” part of those diets that is doing anything?…). Perfect unless you are a dog or cat with pancreatitis. When the pancreas is inflamed dietary fat can stimulate CCK release, contraction of the pancreas and release of digestive enzymes… into the pancreas. This promotes continued autodigestion of the pancreas and surrounding tissues, malabsorption of nutrients, and pain. Cats and dogs with abdominal pain can be very stoic, but if you or a human loved one has experienced pancreatitis you know it is not fun. Fat is sometimes your friend, but sometimes your dog or cat’s worst enemy.
- Digestibility is important for everyone. In general, over-the-counter (OTC) adult maintenance dog and cats food will be less digestible than the therapeutic intestinal support diets sold by veterinarian. This means that more of the OTC diet you feed (yes, even the “premium” priced ones) becomes poop rather than getting absorbed by your dog or cat. There is some variability in OTC diets and a number of the newer “premium” marketed foods, especially ones that are frozen/freeze-dried raw or fresh pasteurized, can be as digestible as intestinal support diets. BUT, before you think that sounds like a great option for animals with pancreatitis, many OTC diets (especially “premium” marketed foods), will have fat contents that exceed 50% of the calories in the diet. These types of diet would be very harmful for a dog with a history or an active case of pancreatitis. OTC diets marketed as “light” or “lean” will have lower fat contents compared to standard adult maintenance foods, but as the fat dropped in OTC diets, so does the digestibility. What about home-cooked foods you may ask? Some combinations of home-prepared foods, like cottage cheese and white rice or chicken breast and white rice, can be as digestible, if not more digestible, than the therapeutic intestinal support diets, but there is going to be a lot more variability depending on the way they are cooked and specific ingredients selected. Also, many home-prepared diets are rarely balanced for long-term feeding ( and if used should only be fed during the recovery stages of pancreatitis (about 2-3 weeks) before your dog or cat is transitioned to a balanced diet whether it is a commercial diet or you have the home-prepared foods balanced for long-term feeding.
- Diet History is key to finding the right diet the first time around. Whenever possible the decision of what to feed and the degree of fat restriction needed should be based on the previous diet intake. This is where diet and treat history are very important. Did your dog (that lovable furry fiend) get into the BBQ remains or a container of bacon grease you’ve been meaning to throw out? In these types of case your dog could have eating a whoppingly high fat intake and as such feeding a moderate fat contenting diet (one that provides between 20-35% fat calories) would be fine. Or did they develop pancreatitis or hyperlipidemia, or both, while eating a diet that was already at 25% fat calories? In this situation, feeding a diet with a similar fat content would not help, and could potentially make them worse. These dogs should be fed a diet that provides less than 20% of the calories from fat. Basically, you want to find out how much fat the dog is eating now and decease it by about half while still staying above the minimum requirement for fat. As I mentioned earlier, cats are a bit different and you want to find a diet that manages whatever concurrent medical conditions your veterinarian finds. Fat triggers and subsequent fat restriction are less important in most cases, but (and I feel like there is always a but) this is not true 100% of the time. I have definitely seen cats in practice that acted more like fat-responsive pancreatitic dogs and needed to fed a highly digestible, fat restricted diet.
The optimal long-term diet choice for a dog or cat with pancreatitis will depend on the inciting cause (genetics, medication, hypertriglyceridemia, or high fat intake) and additional medical issues (diabetes mellitus, IBD, etc). Irrespective of underlying cause, dogs with a history of pancreatitis should never be fed diets or treats with more than 45% of the calories coming from fat due to the risk of recurrent pancreatitis.
Happy and Healthy Feeding!
Lisa P. Weeth, DVM, MRCVS, DACVN
As usual a wonderful and well written article full of all relevant and useful information. Difficult information put in a simple and understandable language. BRAVO!
We, the nutritionists, use the term “Digestible” referring to what animal consumes and excretes. Should we differentiate between “True digestibility which happens in small intestines (ileal digestibility) and Total digestibility which also include fermentation in the large intestine?”
In my opinion, food should be “highly digestible” in small intestines where the nutrients like amino acids, simple sugars, fatty acids, vitamins and minerals are absorbed and subsequently utilized by the body.
Once the useful nutrients (undigested protein, starch and fat) escape into the large intestine, bacteria ferment them either into useful short chain fatty acids or wasteful, and potentially harmful, compounds. Of course! we want soluble dietary fibers to be fermented into SFA.
I feel that the ileal digestibility is more meaningful than the total digestibility.
Would love to hear your viewpoint.
LikeLike
Hi Avi,
Thanks for the feedback! Glad you enjoyed it. 🙂
I agree. What I recommend feeding a “more digestible” or “highly digestible” diet, I’m really refers back to small intestinal (i.e. ileal) digestion and assimilation of the macronutrients protein, fat and carbohydrates. It can be hard to convey the difference between ileal and apparent digestibility to the pet owning public (and even some small to medium sized pet food companies!) and I’ve had a few pet food companies tell me their diets are very digestible but all they’ve collected is Total Digestibility (i.e. diet intake vs fecal collections). As you mentioned, resistant starches, some fats, and undigested protein (the macronutrients that are not digested by the host animal) can be degraded and metabolized by colonic bacteria making the diet ileal digestibility look better than it really is. And create some noxious smelling (and potentially harmful) volatile compounds in the process!
Lisa
LikeLike
Thank you Lisa!
I agree with you.
Due to the non-invasive policy of most of the pet food companies, they can not perform ileal fistula procedure in dogs and cats to determine the ileal digestibility. However, academic institution can and have done that. A few science oriented pet food companies have established “in vitro” systems to determine the ileal digestibility and I understand that those values have correlated very high with the “in vivo” ileal digestibility in dogs. I don’t know if these “true digestible” values have been published.
Anyway, thank you very much for your feedback!
– Avi Deshmukh
LikeLike
I’ve only recently discovered your blog, but I appreciate all of your articles! (Favorites so far: this one, cat nutrition, and kibble chaos). I’ve been in the veterinary field for over a decade, but just recently earned my RVT license. I work at a general practice and we do see a fair amount of pancreatitis cases, usually canine. I knew the basics of the disease and treatment, but this article helped fill in some gaps. Regarding the issue of digestibility: some clients look at the ingredients of a prescription food and balk because to them, it looks like it’s full of “fillers” and very much indigestible. As I’m sure you know, it can be difficult to educate these clients while stressing the importance of feeding the recommended diet following an episode of pancreatitis. Any tips for making client compliance more successful?
LikeLike
Hi Carrie,
Thanks for reading and taking the time to write a comment and question. The World Small Animal Veterinary Association (WSAVA) has some good references and resources from both practices and owners that may come in handy (http://www.wsava.org/nutrition-toolkit) for general nutrition and diet discussions. When it comes to talking to dog and cat caregivers about managing specific disease though I try to keep the focus on the patient and their dietary needs. I talk them through the specific dietary needs (like reducing fat intake and increasing digestibility for cases of pancreatitis) and then we look at different diets that will meet those needs.
I also assure them that everything that is found in the Rx dog and cat foods is highly regulated (more so than OTC diets) and must have some nutritional purpose, so nothing on the ingredient list of a veterinary prescription diet is a “filler” in the sense that is taking up space in the package without any nutritional purpose. Some people will point to ingredients like “powdered cellulose” or “beet pulp” as fillers, but these are being added as either an insoluble (powdered cellulose is often from peanut hulls, which is a great source of insoluble fiber) or mixed soluble-insoluble fiber sources (beet pulp, which is from sugar beets), just like some people take oat bran or ground psyllium husk as fiber supplements in their own diets. If anything these types of ingredients are pretty environmentally-friendly as both peanut hulls and beet pulp are simply “by-products’ of the human food industries that would otherwise end up in a landfill. Over-the-counter diet still have to follow state mandated rules, but some states are more lax in their enforcement than others. I’ve seen a number of smaller labels get away with listing ingredients that have no nutritional value to pets, but appeal to owner’s own food ideas and ideals. These are what I call “label fillers”.
Digestibility-wise, there is a fairly wide range in commercial diets depending on the types on ingredients used, but in general the Rx diets start with ingredients (proteins and carbs) that are more consistently digestible than any diet found OTC (even within the same manufacturing company) and then will add different fibers types and amounts to meet the GI needs of the disease they are targeting. For example, weight loss diets for obese animals often have higher insoluble fiber contents to help the animal feel more full; diets for animals with colitis will have a higher fiber content as well to help reduce fecal water content and modify GI transit; and diets for animals with upper GI problems (vomiting and diarrhea due to maldigestion, whether it is from gastritis, enteritis, or pancreatitis) will have lower insoluble fiber levels but higher soluble fiber (also called prebiotics) levels to help maintain normal floral balance.
Hope that helps!
Lisa
LikeLike